|
|
Stress: Physiological and Immunological Reactions As part of our on-going Q&A about histamine, Dr Janice Joneja was asked whether there could be a connection between chronic hives, stress, anxiety ane histamine. Her answer to that specific question can be found here, but she went on to discuss the physiological and immunological effects that stress can have on the human system. |
|
Stress of all types triggers a complex series of reactions in the body that involve several different endocrine and immune system responses. These responses can result in both beneficial and detrimental effects depending on the processes and consequences of the reactions. The “fight or flight” reaction to immediate danger is obviously extremely beneficial when a person is faced with a life-threatening situation, but such a response as a result of chronic, unrelieved anxiety can lead to very distressing symptoms, ill-health and overt disease. Research is beginning to uncover the complicated pathways of response to different stressful triggers, which we hope will eventually enable us to manage the undesirable consequences of the stress response while still retaining those needed for our safety. I have constructed a rather simplified diagram (Figure 1) to illustrate the important aspects of the stress response and how the endocrine and immune systems interact in different situations. Stress, which may be physical, sensory (e.g. visual, auditory), or emotional, can trigger various physiological pathways:
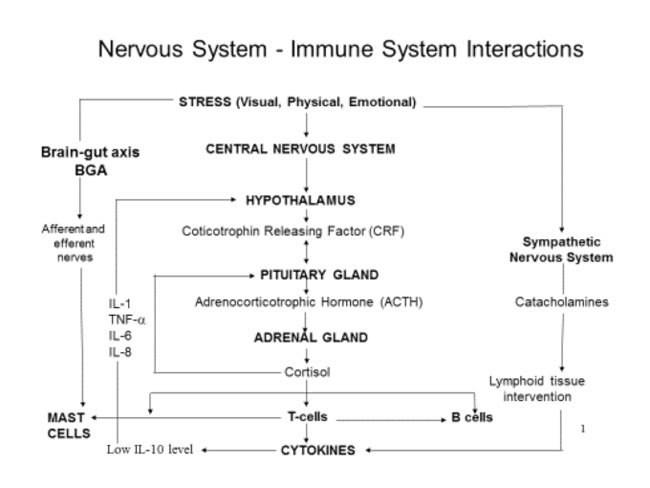
The central nervous system is connected to the immune system by regulatory chemicals. Consequently, stress can result in both suppression and activation of the immune response, resulting in a variety of fluctuating symptoms which may be difficult to diagnose and control. Each of the pathways described above can affect the immune system in different ways. The CNS response results in the generation of cortisol, which can act as an immunosuppressive agent by reducing the proliferation of T-cells, which are essential and central to the protective immune response, and impeding their production and recognition of cytokines, such as interleukins. This suppression of the immune response can render individuals suffering from chronic stress highly vulnerable to infection and other diseases. In contrast, stress can result in activation of mast cells, the leukocytes (white blood cells) in tissues that make and store inflammatory mediators that are released in a protective or allergic immune response. Degranulation of mast cells results in the release of a number of mediators, including heparin, histamine, tryptase, prostaglandins, leukotrienes and other inflammatory molecules. Please see my publications such as “The Health Professional’s Guide…”, “Dealing with Food Allergies” for details of the immune system response and mast cell degranulation. (You can buy all of Dr Joneja's books here in the UK or here in the US.) This reaction is particularly evident in disorders in the digestive tract such as IBS. Histamine indubitably plays an important role in many of these effects, acting in its capacity as a protective agent in the inflammatory response; an important neurotransmitter; and trigger for gastric secretions in digestion. However, in excess, histamine can have extremely detrimental effects – see my article on histamine here. As further research reveals more specific details of the effects of stress, it is hoped that intervention at critical stages in the various physiological pathways, in the form of drugs or other agents, will lead to prevention of the detrimental outcomes that an increasing number of individuals are suffering as a consequence of such factors as genetic inheritance, coping styles and the pressures of modern living. In the meantime it is obvious that the most important remedy for reducing the severity of stress-related disorders and diseases is development of strategies to cope with excessive and chronic stress in all its forms. References: Farhadi A, Fields JZ, Keshavarzian A. Mucosal mast cells are pivotal elements in inflammatory bowel disease that connect the dots: stress, intestinal hyperpermeability and inflammation. World J Gastroenterol. 2007 Jun 14;13(22):3027-30. Gareau MG1, Silva MA, Perdue MH. Pathophysiological mechanisms of stress-induced intestinal damage. Curr Mol Med. 2008 Jun;8(4):274-81 Joneja JM Vickerstaff. Psychological factors and stress in IBS. In: Digestion, Diet and Disease: Irritable Bowel Syndrome and Gastrointestinal Function. Rutgers University Press, Piscataway, New Jersey. August 2004 ISBN 0-8135-3387-2 197-206 Joneja JMV, Ehmann T. Stress profile of clients referred for investigation of food allergy. Journal of Nutritional and Environmental Medicine 2000 10(4):289-296 Joneja JMV, Carmona Silva C. Outcome of a histamine-restricted diet based on chart audit. Journal of Nutritional and Environmental Medicine 2001;11(4):249-262 January 2016 • If this article was of interest you will find many other articles on unlikely allergies and allergy connections here – and links to many relevant research studies here. |












