|
|
Anaphylaxis without warning – could it be buckwheat? Dr Michael Radcliffe is a consultant in the Allergy Service at University College Hospital, London. He describes an unusual case where new-onset food allergy happened for the first time in an adult, whereas most cases of true food allergy (the type that can lead to anaphylaxis) commence in childhood. He discusses possible reasons why this might happen. |
Melissa, aged 42, had a meal at a Japanese restaurant. Whilst eating the meal, her mouth swelled, and she became hot and intensely itchy. Attempts to take water resulted in choking and she briefly lost consciousness. She was blue-lighted to hospital, where she recovered with the help of injection treatment. The A&E department referred her to the allergy clinic for an assessment. She had a history of hay fever, but none of asthma, eczema or food allergy. She had started taking omeprazole (trade name Losec – a prescription-only treatment for reflux and heartburn) a few days earlier but decided to stop it after this incident. Because she had eaten the same meal previously without any adverse effects, Melissa suspected that the omeprazole treatment was the reason for the reaction. What caused the allergy? The ingredient list of the Japanese meal was obtained. The meal had contained chicken, shrimps, egg, yakisoba noodles, beansprouts, peppers, edamame beans, white and spring onions, fried shallots, pickled ginger and sesame seeds. If the meal had contained a rarely encountered food allergen, then this would have been the most likely culprit. Our first thought was the edamame beans, but the allergy clinic dietitian informed us that edamame means soya, a possible culprit nonetheless. Skin prick tests to soya bean, shrimp/prawn and sesame seed were undertaken, but the results were negative. However, it turns out that a rarely encountered allergen was present. We had assumed that yakisoba noodles were made of wheat but discovered that yakisoba is Japanese for ‘fried buckwheat’. We undertook skin prick and allergy blood tests for buckwheat, and both were positive. Unknown in the UK as a food allergen until about fifteen years ago, cases of allergy to buckwheat are now being seen in UK allergy clinics and buckwheat allergy is becoming increasingly recognised across Europe. However, buckwheat has yet to be added the list of foods and food groups required to be declared on the label of pre-packages foods in the European Union. 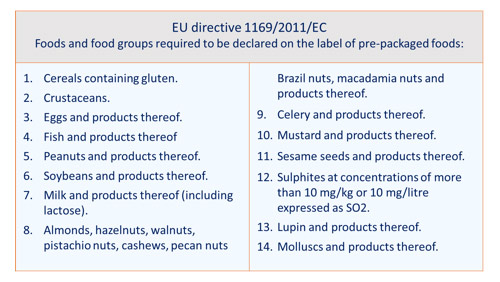
But the situation in Japan and Korea is very different. Buckwheat is amongst the food allergies most commonly diagnosed and a possible explanation has been proposed. In both Japan, Korea and other southeast Asian countries, there is a long tradition of using buckwheat husk as a filling for pillows. Sensitisation via inhalation Food sensitisation (the immune event that results in allergy) mostly occurs in infancy and it either happens following food ingestion, or following contact with inflamed skin, for example when food comes into contact with inflamed or damaged skin in an infant with eczema. In contrast, most newly-arising food allergy in adults occurs following the inhalation of tiny particles of a food that contains the responsible protein (the allergen) or an item (e.g. pollen grains) that contains the same protein. Most food allergens do not cause sensitisation in this way, but buckwheat is one of those that can. This why buckwheat pillows are likely to be a major cause of buckwheat allergy in the Far East. A short while after being given the bear, she developed hay-fever-like symptoms and, realising that the bear was the cause, she disposed of it and the symptoms disappeared. When she consulted her GP, it was suggested that allergy to mould spores was the likely reason for her symptoms. It was only after she was later diagnosed with buckwheat allergy that she realised the true cause. Another case of buckwheat allergy was reported in the British Medical Journal in 2011. A 63-year-old female was referred for assessment of an allergic reaction to a new brand of muesli. It contained oat, raisins, sultanas, currants, sunflower seeds and buckwheat. Within minutes of eating, she developed a wheezy cough and widespread urticaria (hives). She attended A&E for treatment and observation and later investigation identified the cause as allergy to buckwheat. She then remembered having suffered from a dry cough and itchy palms when shelving buckwheat flour while working at a supermarket a few years earlier. Could there be another explanation? The possibility that inhalation of buckwheat dust or buckwheat flour might have resulted in buckwheat allergy in Melissa’s case was re-considered. However, Melissa considered this to be unlikely and so we re-examined her own theory that the antacid treatment could have been responsible.
A study on mice supports this theory. Two groups of mice were each fed fish protein (a food they had not eaten previously) every day for 3 months. The first group were taking omeprazole treatment whilst the second group were not. The first group produced fish protein antibodies whilst the second group did not. June 2018 • If this article was of interest you will find many other articles on unlikely allergies and allergy connections here – and links to many relevant research studies here. |

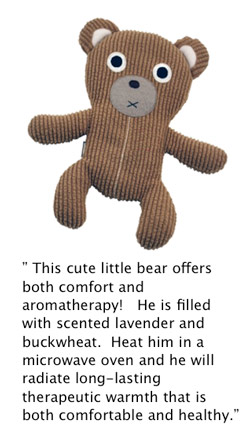 In the UCLH allergy clinic we have seen two cases of newly arising buckwheat allergy where sensitisation was likely to have occurred via the respiratory tract. One was linked to use of a buckwheat pillow (buckwheat pillows have recently become popular in the UK), and the other case concerned a teenager who suffered severe anaphylaxis whilst eating a buckwheat pancake containing hazelnut spread. Doctors advised her that buckwheat did not cause allergy and that hazelnut was the most likely cause of the attack. She then suffered a further attack when she ate another buckwheat pancake which did not contain hazelnut. She then remembered that about a year previously she had been given a buckwheat-stuffed, lavender-scented, cuddly bear which included the instruction to heat it in a microwave prior to cuddling and inhaling the fragrance.
In the UCLH allergy clinic we have seen two cases of newly arising buckwheat allergy where sensitisation was likely to have occurred via the respiratory tract. One was linked to use of a buckwheat pillow (buckwheat pillows have recently become popular in the UK), and the other case concerned a teenager who suffered severe anaphylaxis whilst eating a buckwheat pancake containing hazelnut spread. Doctors advised her that buckwheat did not cause allergy and that hazelnut was the most likely cause of the attack. She then suffered a further attack when she ate another buckwheat pancake which did not contain hazelnut. She then remembered that about a year previously she had been given a buckwheat-stuffed, lavender-scented, cuddly bear which included the instruction to heat it in a microwave prior to cuddling and inhaling the fragrance.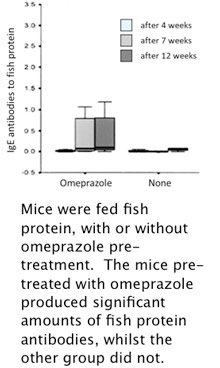 Omeprazole is a powerful antacid that can reduce gastric acidity from pH 2 (normal) to pH 5. Although this relieves the acid-related symptoms, at pH 2, gastric protease enzymes break down proteins intoamino acids, whereas at pH 5, they do so incompletely. This increases the likelihood that sensitisation might occur when cells of the immune system becomes exposed to partially intact proteins across the gut wall.
Omeprazole is a powerful antacid that can reduce gastric acidity from pH 2 (normal) to pH 5. Although this relieves the acid-related symptoms, at pH 2, gastric protease enzymes break down proteins intoamino acids, whereas at pH 5, they do so incompletely. This increases the likelihood that sensitisation might occur when cells of the immune system becomes exposed to partially intact proteins across the gut wall. 










